EM PROGRAM OVERVIEW
What sets Hennepin EM apart?
Hennepin EM residents train in a busy, urban ED with over 100,000 patient visits per year. Our primary hospital, Hennepin County Medical Center, is a Level 1 Adult and Pediatric Trauma Center and a mission-driven hospital, caring for a diverse and underserved patient population. We recognize that patient care requires more than medical knowledge, and our training program will provide you with the leadership, communication and systems knowledge to practice medicine successfully in a wide variety of settings.
The Emergency Department is located on the main HCMC campus, which spans five city blocks in downtown Minneapolis, next to the new US Bank Stadium and Downtown East Commons Park. HCMC provides the entire spectrum of care for injured or ill patients, from pre-hospital care through rehabilitation. The Emergency Department is divided into three team centers: Team Center A with 15 high-acuity patient beds, Team Center B with 11 moderate-acuity patient beds, and Team Center C with 12 beds for pediatric patients or lower acuity complaints.
The Pit-boss Role
Hennepin County EM provides the unique opportunity for senior emergency medicine residents to supervise and coordinate patient care across the different team centers. During the first and second year, residents serve as a primary medical providers (PMPs) for patients. In Team Centers A and B, PMPs staff their patients with a third year resident “Pit Boss”. Pit Boss shifts (about 80% of third-year shifts) are spent running stabilization cases, managing and coordinating care for all of the patients in a 12-15 bed Team Center, and directly supervising PMPs, which include EM residents, off-service rotating residents, physician-assistants, and medical students. All stabilization cases are managed by Emergency Medicine senior residents with faculty supervision.
From day one, residents assume critical decision-making responsibilities in a supportive, collaborative, and fast-paced environment. Residents interact with dedicated faculty and provide care to a diverse population that includes both urban and underserved individuals, as well as trauma patients from across Minnesota and neighboring states.
Procedural Training
Hennepin County EM has provided cutting edge procedural training for Emergency Medicine residents since 1972. Emergency Medicine residents perform all procedures in the ED, including intubations, central lines, fracture/dislocation reductions, lumbar punctures, thoracotomies, chest tubes, etc. Additionally, residents go through two separate procedural workshops each year, one for routine EM procedures, and a separate cadaver-based lab for resuscitative procedures. These are taught by faculty using a one-to-one student/teacher ratio.
Emergency Department Facts
- Level I Adult and Pediatric Trauma Center, Stroke Center
- More than 100,000 ED visits and over 72,000 ambulance runs annually
- Includes 57 examination rooms and four stabilization rooms
- Over 20 mobile ultrasound machines with wireless connectivity plus mounted ultrasounds in stabilization bays
- 2 dedicated CT scanners and complete digital medical imaging system
- Newly renovated triage area including 8 fast-track treatment rooms
- Dedicated resident work area
- Electronic Health Records and fully integrated Epic system with Dragon dictation available
Ultrasound
Hennepin County EM is simply unmatched when it comes to emergency ultrasound. HCMC was the birthplace of emergency point-of-care ultrasound in 1985, when HCMC faculty began authoring some of the first publications describing how emergency physicians can use point-of-care ultrasound to improve patient care. Each stabilization bay has a mounted Mindray TE7 touchscreen ultrasound machines and the various team centers share over 20 mobile US machines. As interns, Emergency Medicine residents work one-on-one with am EM Ultrasound Education Technologist to learn the basics of EM point-of-care ultrasound, during two dedicated Ultrasound weeks.
Cutting Edge Curriculum
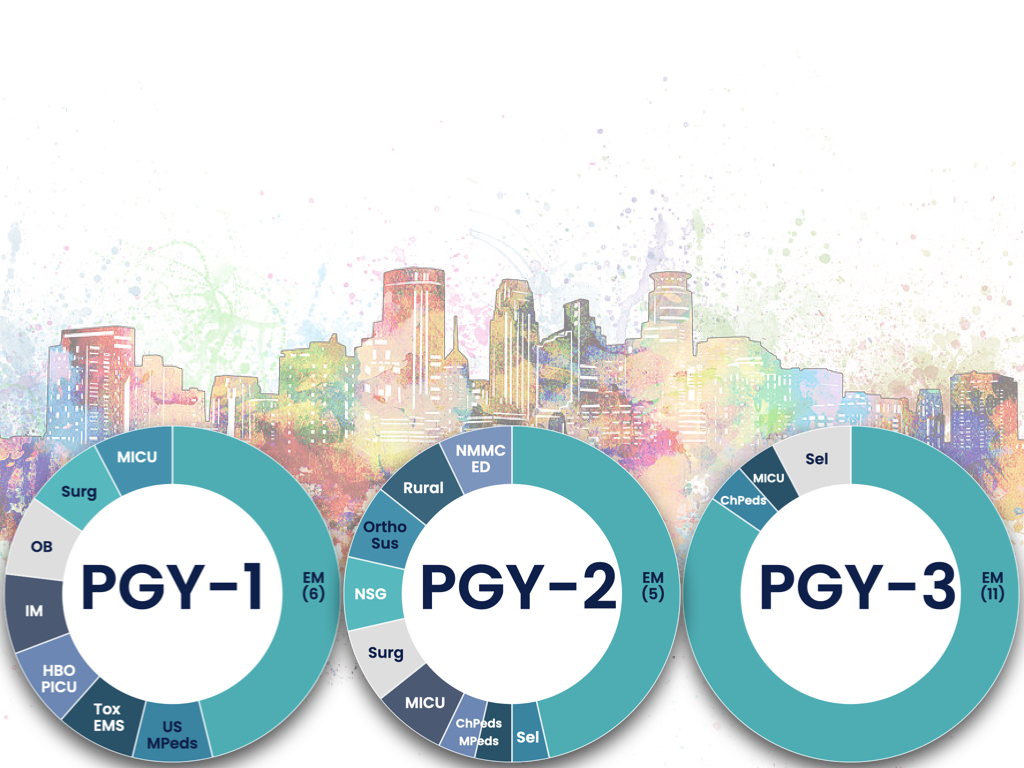
Hennepin County EM has placed as much effort into its didactic curriculum for EM residents as it has into its world class clinical training. Core EM content is presented during our weekly Thursday EM Conference Day. The morning starts at 7am with Stabilization and Critical Care Conference, presenting the most challenging cases of the week to highlight the important lessons to be learned in the management of critically ill or injured patients. The rest of the conference morning is broken up into 30-60 minute sessions. Careful attention has been paid to encourage an active learning environment, so that residents get the most out of each minute of conference. At noon, EM interns regroup for “Reading Group”, a chance to review the basics of EM from a “chief complaint” perspective, and walk through some of the required readings and landmark articles in Emergency Medicine. Additionally, residents have a simulation-based High-Acuity/Low Frequency curriculum, where three-times per year, residents try to work through some of the most complicated critical care they will encounter, all based on real cases. These educational sessions are always protected, and residents are almost always able to attend, even when rotating on off-service rotations. The three-year rotation structure is constantly fine-tuned to provide EM residents with only the most high-yield experiences as they progress as residents. The current structure is displayed below.